For a colonoscopy, the preventative care coverage under the Affordable Care Act means that the doctor is covered. What about the exam center? Is it covered? What about any anesthesia and anesthesiologist? What about the prescription liquid stuff I have to drink before to cleanse my colon? What about the initial visit to the doctor before my procedure?
Answer
For most preventive services, only the screening itself is covered at no charge. The actual services required can be subject to cost sharing, and that is based on what plan you have or in many cases, how the doctor's office bills your insurance.
All ACA-compliant private Major Medical plans (including Marketplace plans) cover the costs for colonoscopy as a screening test, patients may be charged for some services. You may have to pay part of the costs of anesthesia, bowel prep kit, pathology costs, and a facility fee (where the procedure is performed).
Colonoscopies that are done to evaluate specific problems, such as intestinal bleeding or anemia, are usually classified as diagnostic – and not screening – procedures. If that’s the case, you may have to pay any required deductible and copay. The same is true if the colonoscopy was done after a positive stool test (such as the FOBT or FIT) or an abnormal barium enema or colonography. Some insurance plans also consider a colonoscopy diagnostic if something is found (like a polyp) during the procedure that needs to be removed or biopsied.
Before you get a screening colonoscopy, ask your insurance company how much you should expect to pay for the exam. Find out if this amount could change based on findings during the procedure. Learn more at cancer.org.
Rule of Thumb: Preventive care visits are generally covered at no cost if they are evaluating your current health status when you are symptom free. Medical treatment for specific health conditions, on-going care, lab or other tests necessary to manage or treat a medical issue or health condition are considered diagnostic care or treatment, and are NOT considered preventive care.
TIP: In order to get your free annual wellness visit, you have to make sure your doctor codes it correctly. You can generally ask your doctor and insurer what each service will be coded as. This allows you to find out if a service will be billed as preventive care or not.
Updated 7/20/2019:
While the Affordable Care Act includes free preventive procedures like colonoscopies, we’re hearing more and more that people are being asked to pay, from community members. We don’t know anyone who keeps overall records on how big this problem is, but we can tell from this article by being one of our busiest posts.
Under the Affordable Care Act, services recommended by the U.S. Preventive Services Task Force are covered with no out-of-pocket payments. For people between 50 and 75, the task force recommends screening for colorectal cancer using stool testing, sigmoidoscopy or colonoscopy. According to the law, if a polyp is discovered and removed during a screening colonoscopy, there will be no charge, because that’s considered part of a routine colonoscopy.
So: screening colonoscopies are supposed be free if you’re in that age group. Diagnostic colonoscopies (in which the provider is looking for a diagnosis for something like stomach pain) are not free; they’re a “sick person” visit.
More than 15 million colonoscopies are performed annually in the United States. Roughly half of them are screening colonoscopies. How many of those incur some charge? A fair number, anecdotally.
PRICES ARE ALL OVER THE MAP
The prices vary widely: We’ve found as little as $600 all in, and as much as $8,000 or even more (see chart at bottom).
There are links to our detailed price lists in this post from clearhealthcosts.com .
Here are examples from our community members’ reporting:
Charge of $3,200; individual paid $370.41: “$3,200 was billed … and $2,331 was the ‘allowed amount’ under my health care plan …. However, I received a separate bill from my doctor who performed the procedure for $800 and the ‘allowed amount’ by my insurance was $370.41 which went to my deductible…. because they found a polyp the procedure coding changed from preventive to diagnostic, therefore, I was no longer covered under preventive care….”
Charge of $8,000; individual paid $800: “I spoke to the CEO of the surgical center. He agreed the fee was high but said there is a standard list of prices that he and most centers adhere to.”
Charge of $2,312; individual paid $844: “Was charged three initial different fees, for MD, facility, and lab work, all reduced … via contract, not payment: (a) 426, reduced to 285; (b) 1400, reduced to 279, and (c) 486 reduced to 280, thus $2312 overall reduced to $844, zero by carrier.”
Charge of $5,104; individual paid $1,650: “I called Kaiser before the procedure to inquire how much it would cost me…. They were vague and would not give me a fixed price, but I was told if there were no special circumstances (in the end, it turned out there were none), it would be around $600 on my plan. Imagine my surprise when I received a bill for $360 for Professional Services, and $1,290 for the hospital bill (my share of each), for a total of $1,650 out-of-pocket. I am on a high-deductible plan, so I paid for 100% of my share.”
Charge of $2,722, insurance paid $743, individual paid $1,979: “I did not ‘shop around’ when I did this. I’m embarrassed to admit that it hadn’t occurred to me to do that. This price check concept is a wonderful service and eye opener for the public. Many thanks.”
SO WHAT CAUSES THIS? HOW CAN THIS BE TRUE?
We’ve heard a handful of explanations. To be sure, a preventive or screening procedure is supposed to be free, and a diagnostic one (a sick person visit) will not be.
1. For some insurers, we are told, if you had a screening colonoscopy before and you had polyps removed, all subsequent colonoscopies will be considered diagnostic and not preventive. In pretty much every one I’ve heard of, something was removed and tested, so that means the first one is free — and none of the rest are.
So you might expect a screening colonoscopy, and learn only later that the insurance company considers it a diagnostic procedure. The letter to me from my gastroenterologist at right doesn’t suggest there will be a charge — but if I had an insurer who follows this practice, it would be an invitation to a sick-person visit and a hefty bill.
2. Some insurance companies will not cover the facility fee, or will cover only part.
3. We have heard of several cases in which the anesthesiologist was out of network, and billed accordingly. So you might have an in-network doctor who uses an out-of-network anesthesiologist, which you learn of only when you get the bill.
4. Billing confusion: “The most common scenario is when it is billed as diagnostic rather than preventative,” Rebecca Palm, Chief Strategy Officer & Founder of copatient, a consumer healthcare expense management company (www.copatient.com) wrote in an email answer to my question about this. “This can happen if the patient has had a previous test that indicated that a colonoscopy should be performed, or if the patient has symptoms that the provider is trying to diagnose.” She added, “Some providers will also code a colonoscopy as diagnostic if it begins as a preventative screening and, while performing the procedure, they discover and remove a polyp.”
5. That mysterious thing that happens in claims processing. We hear all the time that providers (doctors and hospitals, for example) have to follow different rules for different insurers that may be confusing, or may change.
Palm said: ‘The way that insurers process these codes varies widely. Some insurers require certain coding modifiers to pay the claim as preventative, while others don’t have the capability to distinguish between those codes. If this happens, you can request that the provider code the procedure differently or that the insurer process the claim as preventative based on the coding rules.”
A friend who knows about this process adds: “If there’s a problem & it’s not clear, it has to be processed as diagnostic & not preventive. I’ve fought claims on that for people even on something that wasn’t straightforward, something like the doctors wanting additional images or views or unclear pictures because of dense tissue in the body made them less than clear; where an immediate problem isn’t exactly found & all of it has to be considered diagnostic still.”
So yes, the coding part is mind-numbing. If you don’t believe us, look at this article on the subtleties of coding.
DON’T BLAME THE AFFORDABLE CARE ACT
The Affordable Care Act is not the cause of this; it’s the product of unintended consequences.
Preventive screenings (including colonoscopies) were made free under the A.C.A. Providers of such screenings, of course, saw an opportunity for increased business. These screenings are suddenly quite heavily marketed (see my gastroenterologist’s letter above).
The problem of surprise out-of-network bills is not a new one, of course. One study estimated that 40 percent of out-of-network bills came as a surprise.
THE TAKEAWAY: QUESTIONS TO ASK
As we always say, know before you go. As a preliminary step, know what’s in your insurance plan.
First, make sure it’s a preventive (screening) colonoscopy. If it’s not preventive (screening) but rather a diagnostic colonoscopy — looking for a diagnosis for a symptom in your GI tract, then it can be charged as a “sick person” visit — just as a screening mammogram is covered under preventive care with A.C.A.-compliant plans, but a diagnostic one is not.
Questions to ask:
- What all is covered? Doctor’s fee, anesthesiologist, lab fees, office visit for preparation, anything else?
- Will there be a facility fee? Does there have to be, or can it be done at another place without a facility fee?
- What kind of anesthesia are you planning to use? How much will it cost?
- Some places choose to pay only for “twilight” anesthesia, while others want full general anesthesia. Do I have a choice, and what’s the price difference?
- If there is a separate anesthesiologist, is that person part of my network (if you’re insured)?
- Will all lab tests be done at a participating lab?
- Do you require a pre-procedure consultation? How much will that cost? Is it mandatory?
- How about the stuff you have to take to empty your system before the procedure? How much is that going to cost? is it covered by insurance?
Take notes, and take names and phone numbers. If you need to question a bill later, it’ll be much easier.
Hospitals and other facilities do not police this as carefully as they might in many cases, and after the fact — even with a huge argument — it’s not always possible to get covered. Many insurers will take the position that it’s your fault, even if you did everything you could to protect yourself. But your case will be stronger if you ask up front, get commitments and assurances in writing, and take names and phone numbers.
Also, we don’t give medical advice, but our friends over at the American Board of Internal Medicine Foundation do, via their Choosing Wisely campaign. Here is a fact sheet on colonoscopies from them.
No, you cannot be charged for a pre-colonoscopy consultation after a screening colonoscopy.
No, you cannot be charged for any lab tests after a screening colonoscopy.
Other resources: Here’s a National Women’s Law Center fact sheet on what to do if you think you’re being charged when you shouldn’t be.
Here’s a Kaiser Family Foundation paper with a set of scenarios for coverage, dating to 2012 (some clarifications have been issued since then, but this is pretty thorough).
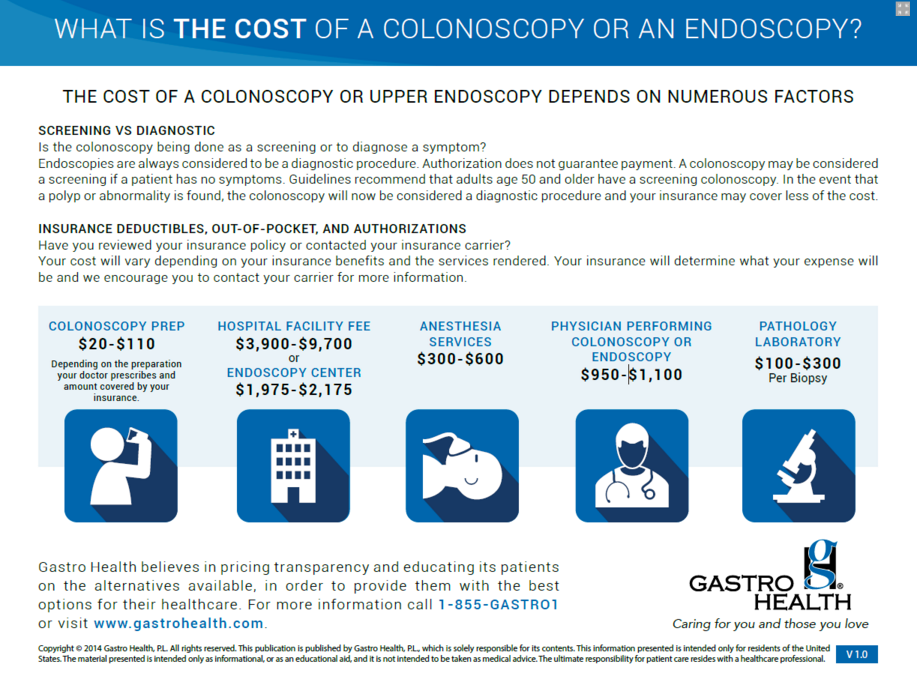
And finally, here’s a sheet from a provider listing the range of prices. While the facility fee is scary ($1,975 to $9,700? come on!), we also want to point out the fee for the “prep” stuff: Here’s a blog post about a person who found out that the cost could be $12.11 without his insurance, or $38 with. I guess he should feel lucky that he wasn’t charged $110.


Comments
6 comments
This isn't correct. Subsequent to passage of ACA, the Dept's of Health and Human Services, Labor, and Treasury issued a series of FAQ's to clarify coverage of preventive services. In general, anything that is considered as being an integral part of the service itself is also covered fully with no cost sharing. In the case of colonoscopy, the pre-surgical consult, prep, anesthesia, polyp removal and associated pathology tests should all be covered by all non-grandfathered commercial and ERISA plans (Medicare plans incur co-insurance for polyp removal).
Q7 from May of 2015 addresses anesthesia: https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/Downloads/aca_implementation_faqs26.pdf
Qs7 and 8 from Oct 2015 address the pre-surgical consult visit and pathology on polyps that are removed during a screening colonoscopy :https://www.dol.gov/sites/default/files/ebsa/about-ebsa/our-activities/resource-center/faqs/aca-part-xxix.pdf
And Q1 from April of 2016 addresses bowel prep: https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/Downloads/FAQs-31_Final-4-20-16.pdf
While diagnostic tests for symptomatic patients do incur cost sharing, many plans, including some Medicare Advantage plans, will also waive cost sharing for colonoscopies that are done as screening to follow up on a positive stool test (i.e.,they are considered part of the screening continuum, not diagnostic).
Thank you very much Andy Cobb. I recently went in for my first routine colonoscopy. Dr. and outpatient center were all in my network on my insurance with Cigna. I went in had it done and had 3 polyps removed. Received a bill 2 weeks later for me to pay 2,190.00 and the total for the procedure that was done in an outpatient hospital in Okaloosa county Fl. was a mind blowing $25,991.00. I was completely in shock. My insurance company sent the hospital a check for over 22,000.00. And my part is 2,190.00. I can not even believe this. And I called the place and they told me maybe there was problem with the coding. I never heard back. A week later I called back, I was put on hold, on and on. Too long of a wait. Called again when I had more time, finally got someone and they told me the removal of the polys was the reason for the cost. I was there less than 2 hrs. Most of that time was sitting on a stretcher waiting to go in for my 20 minute procedure. They told me I still needed to pay the above. Thanks to your information I will be adding it to my claim to not pay this crazy amount. They have already been over paid by my insurance company. They were paid enough for 5 or 6 people to have had Colonoscopies with surgery. Thanks again for this important information.
DEBRINAMARIA, I'm so sorry you're having to deal with this. $25K for a colonoscopy is ridiculous, even with polyp removal. There's no transparency into contracted rates between providers and insurance companies, but that's 10x a reasonable amount. Still, the best thing you can do is focus on the balance they are billing you.
First, contact Cigna to address this. If you're getting this plan through your employer or on the exchange and it's not grandfathered (Cigna can tell you what kind of plan you have when you contact them), they should cover this at 100% and can help adjudicate this with the doctor's office. If that doesn't get you anywhere, you still have a couple of options.
Hopefully you can get this addressed without getting to the last 2 points. I do think many of these cases are just miscoding and a lack of incentive for either doctor's offices or insurance companies to address the problem, rather than anyone being malicious. Unfortunately it leaves patients stuck in the middle, and the only way to really create incentive is to push back. I'm rooting for you!
Andy Cobb, thank you especially for the link on anesthesia. I had a colonoscopy screening in November, 2019. The insurer has stated I am obliged to pay $528 for part of the anesthesia bill and anther $1200 for part of the recovery room bill. I have formally appealed to the insurer for both the anesthesia charge and the recovery room charge. I found your phrase "integral part of the service" interesting. As I bet you know, the phrase (or similar wording) appears in CMS documents but not the ACA text itself. Do you or anyone here have knowledge of the recovery room being considered an "integral part of the service" in the case of a colonoscopy? Would a doctor let a patient skip the recovery room? Of course I did not know enough to ask whether I had a choice to do so. The damned staff must have been salivating at everything they got to bill me.
I try to keep my emotion out of my communications with the insurer and provider. If the insurer denies my appeal, then I am ready to elevate my appeal to the state insurer.
I had a colonoscopy five years ago and paid not one dollar for it. I was led to believe that the November 2019 colonoscopy would likewise cost nothing. I am disgusted with the lack of transparency. But I admit that, with a little more enlightenment, I could have asked questions directly of the insurer.
Lesson learned. Do not trust the medical facility, its staff, the doctor, or any vague verbiage in the insurance plan. Meanwhile, the mere fact that the insurer is billing me in part for the anesthesia (for now) tells me the company is crooked.
Update, March 17, 2020:
A couple of weeks ago I went to the provider and asked for a copy of all documents that were reviewed by me and others for my November colonoscopy. The provider staff were great. One of the documents indicated that the day of the colonoscopy, the provider communicated with my insurer. In writing, the insurer's representative said there was no co-pay, no charge, nothing to be billed to the patient. A second document indicated that there might be additional charges for anesthesia and other services. But this second document had a space for the patient's (my) signature. I had not signed it, and I do not recall seeing this second document the day of my procedure or at any time. I took the copies, scanned them, and submitted them as addendums to my appeal to my insurer. Today I received a letter from my insurer saying that the insurer would be paying for all the costs of the colonoscopy (doctor's bill; recovery room; anesthesia; the whole enchilada).
This site was way helpful. Thanks in particular to Andy Cobb.
my husband suffered from crohn's disease almost all his life and i can tell you that its really terrible, watching him get lean and pale worried me the more, he lost appetite, he was always and was unable to go to work again,he kept having sores in his mouth and the constant pain was making the situation worse. we kept going from one gastroenterologist to another, they were not helping the situation, they kept giving us different drugs and it was making it worse,they kept increasing the dosage, in 2016 when i went to cvs pharmacy to go and get another drugs for him, that was were i heard about dr folonsho a herbal doctor, who specialises in using natural roots and herbs to treat diseases and chronic pain. at first i was in doubt, because we have tried many options that were not helping and all the doctors we came across told us that there was no cure, and i believed, so i contacted this herbal doctor and he said he could help my husband,after i told him my problem, he said he has a herbal remedy that can heal my husband and reverse this illness completely and he will be back to his normal state of health, not having many alternatives anymore i requested for the herbal remedy,because the situation ws getting worse, after using the medicin for about 3 weeks there was great improvement, and my husband was getting back to his normal self, its been 4 years now and my husband is still strong as ever, all thanks to dr folonsho, and may GOD continue to bless you, so if you are still sufferring from this disease kindly ciontact dr folonsho today either through email drfolonsho@gmail.com or via whats app +2348073410606 or you can check out his website https://drfolonshoherbalhome.simdif.com/ and you will be glad you did, i wouldnt want someone to experience what my husband experienced
Please sign in to leave a comment.